What is Vaginitis?
Vaginitis is an inflammation or infection of the vagina, which causes discomfort, itching, and discharge. It can occur due to an infection, or due to a change in the vaginal ph. It can also occur after the menopause due to thinning of the vaginal tissues. In some cases, it can be caused by allergic reactions to vaginal sprays, douches or creams.
Causes of Vaginitis
Vaginitis can result from various factors, including:
Infections: The most common causes are due to yeasts and bacteria.
- Yeast, to some extent, is a common part of the vaginal flora. But it can flare up and increase to cause vaginitis. The most common yeast is usually Candida albicans
- Bacteria – Bacterial infections like Gonorrhea and Syphilis are sexually transmitted diseases.
- Virus – Viruses like Herpes Simplex and Human Papilloma virus ( virus) can cause vaginitis with itching and formation of blisters ( with HSV) and growth of warts (with HPV)
- Parasites – Parasites like Trichomoniasis can cause severe vaginitis with severe itching and a large amount of frothy vagina discharge.
Change in the vaginal ph
A change in the vaginal ph can lead to a condition known as Bacterial Vaginosis (BV). BV is not exactly an infection. It occurs when a normal bacteria in the vagina called Gardnerella increases in amount to cause symptoms.
Chemical Irritants
Products such as soaps, bubble baths, douches, and spermicides can irritate the vaginal tissues.
- Hormonal Changes: A drop in estrogen levels, especially during menopause, can lead to thinning of the vaginal lining, resulting in inflammation. This condition is known as Postmenopausal vaginitis or Atrophic vaginits.
- Allergies: Some women may have allergic reactions to certain products like latex in condoms or ingredients in personal care products. foreign objects, such as toilet paper or forgotten tampons, in the vagina can also cause allergic reactions.
- Sexual Activity: New sexual partners or multiple partners can sometimes increase the risk of infections that cause vaginitis.
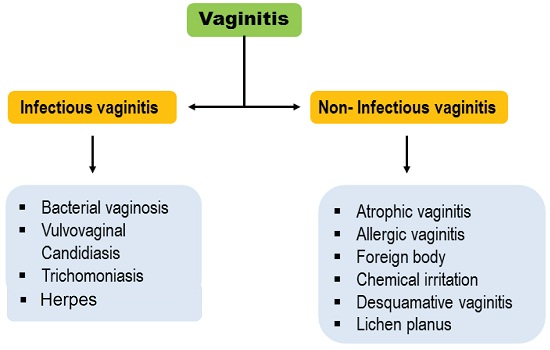
What are the common types of Vaginitis?
There are several types of vaginitis, but some are quite common:
- Bacterial Vaginosis (BV): BV is not really an infection. But it causes all the symptoms of an infection due to overgrowth of normal vaginal bacteria like Gardnerella. The normal environment of the vagina is maintained by the vaginal ph which is usually slightly acidic. Bacteria like Lactobacillus help to maintain this ph. But if the vaginal ph changes due to any cause like stress or any infections, then the ph can change. This allows excessive growth of Gardnerella causing an imbalance of the natural bacterial flora in the vagina. BV is one the most common type of vaginitis among women of reproductive age.
- Yeast Infection (Candidiasis): Like Gardnerella, yeast is also a normal part of the vaginal environment.The vaginal ph maintained by lactobacillus act to prevent an overgrowth of yeast. But that balance can be disrupted if lactobacillus decreases due to any cause. Overgrowth of yeast occurs with the typical symptoms of itching and vaginal discharge.
- Trichomoniasis: Trichomoniasis is a sexually transmitted disease. It is caused by a parasite Trichomonas vaginalis. In males, it may not cause any symptoms but in women, it can cause intense itching with an increased vaginal discharge.
- Herpes Genitalis Infection: HSV is a virus which spreads readily between sexual partners, especially if one of them have an active infection at the time or sexual intercourse.
- Atrophic Vaginitis: Also called postmenopausal vagnitis, it occurs due to less estrogen in the blood after the menopause. The decreased estrogen causes thinning of the vaginal cells which causes them to be easily susceptible to infection like yeast or BV. Atrophic cells can be very itchy even without an active infection.
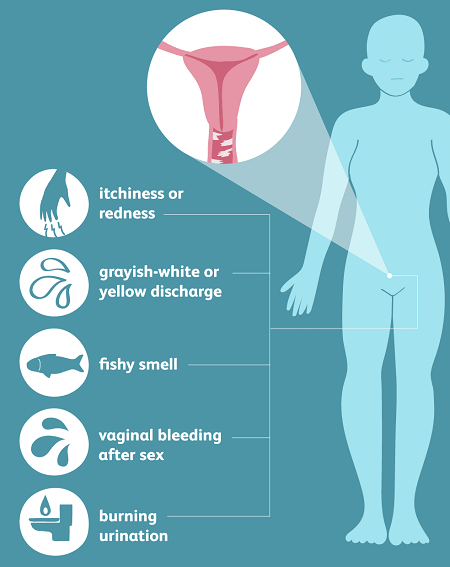
Symptoms of Vaginitis
The symptoms of vaginitis can vary depending on the type of infection, but common signs include:
- Discharge: Unusual discharge that might be white, gray, yellow, or green and can have a different consistency or smell.
- Itching: Persistent itching in and around the vagina.
- Odor: A strong, unpleasant vaginal odor.
- Pain: Discomfort or pain during intercourse or urination.
- Sores: There may be blisters or sores in the genital area
- Redness and Swelling: The vaginal area might be red, swollen, or irritated.
How is Vaginitis diagnosed?
Vaginits caused by yeast or BV can generally be diagnosed from symptoms and by physical examinations. But lab tests may be needed for confirmation, especially for vaginitis caused by sexually transmitted diseases.
- Medical History: You will be asked about your symptoms, sexual activity, menstrual cycle, and any products you use that might irritate the vagina.
- Physical Exam: This includes a pelvic exam to look for signs of infection and irritation in the vagina or around the internal organs like the uterus and ovaries.
- Lab Tests: A sample of vaginal discharge may be taken to identify the type of infection or to rule out other conditions.
Risk Factors
Certain factors can increase your risks of developing vaginitis:
- Sexual Activity: Having new or multiple sexual partners can increase the risk of infections.
- Hormonal Changes: Pregnancy, menopause, or using hormonal contraceptives can alter the vaginal environment.
- Medications: Antibiotics and steroids can disrupt the natural balance of bacteria in the vagina.
- Personal Hygiene Products: Using douches, scented tampons, or feminine sprays can irritate the vagina.
- Diabetes: Poorly controlled diabetes can increase the risk of yeast infections.
Treatment of Vaginitis
Treatment depends on the type of vaginitis:
- Bacterial Vaginosis: BV is typically treated with antibiotics, either oral or topical.
- Yeast Infection: Antifungal medications, available as creams, ointments, tablets, or suppositories, are used to treat yeast infections.
- Trichomoniasis: This is treated with a specific antibiotic called metronidazole or tinidazole.
- Viral Vaginitis: Treatment focuses on managing symptoms and may include antiviral medications if caused by herpes.
- Non-Infectious Vaginitis: Avoiding the irritants that caused the problem is key. Your doctor might recommend topical corticosteroids to reduce inflammation.
- Maintenance of vaginal ph: It is most important that you are given treatment to maintain the vaginal ph. Boric acid suppositories can help make the ph acidic and prevent growth of yeast or Gardnerella. You will also need to take probiotics to increase growth of lactobacillus.
Complications of Vaginitis
While vaginitis itself is usually not serious, complications can arise if it is left untreated:
- Pelvic Inflammatory Disease (PID): Untreated BV or trichomoniasis can lead to PID, a serious infection of the reproductive organs.
- Increased Risk of STIs: BV and trichomoniasis can increase the risk of contracting sexually transmitted infections, including HIV.
- Pregnancy Complications: Pregnant women with untreated BV are at risk of preterm delivery and low birth weight babies.
- Chronic Discomfort: Persistent symptoms can lead to ongoing discomfort and stress.
Prevention of Vaginitis
Prevention of vaginitis is very important. Prevention is always better than being treated for the condition:
- Practice Good Hygiene: Wash the vaginal area with mild soap and water. Avoid douching, which can disrupt the natural balance of bacteria.
- Wear Appropriate Clothing: Choose cotton underwear and avoid tight-fitting clothes that can trap moisture.
- Safe Sexual Practices: Use condoms to reduce the risk of STIs and limit the number of sexual partners.
- Healthy Lifestyle: Maintain a balanced diet, manage stress, and control blood sugar levels if you have diabetes.
- Be Careful with Products: Avoid using scented products, harsh soaps, and other potential irritants around the vaginal area.
- Regular Check-Ups: Regular gynecological exams can help detect any issues early on and keep you informed about your vaginal health.
Vaginitis is a common and usually manageable condition. It can be prevented to a great extent by taking precautions to minimize risks. If not, it can be treated with medicines.
Read More Questions and Answers on Pregnancy and Gynecology
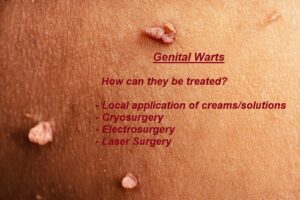
How are Genital Warts treated?
Genital Warts are caused by the Human Papilloma Virus (HPV) and is one of the most common sexually transmitted diseases.
Birth Control methods
Birth Control methods like pills, patches, condoms and IUDs are temporary methods. Permanent methods are tubal ligation and vasectomy. Emergency contraception like pills and Copper Ts are also important.
Vaginitis Symptoms, Causes & Treatments | Expert Guide by Dr. Madhumita Mazumdar
Vaginitis is an inflammation of the vagina causing symptoms like abnormal vaginal discharge, itching, pain and swelling. It is usually caused by a bacterial or fungal infection.

Sexually Transmitted Diseases -Types, Causes, Spread, Symptoms and Treatment
The common STDs are Syphilis, Gonorrhoea, Chlamydia, Trichomoniasis. Hepatitis B, Herpes simplex virus (HSV), HIV and Human papillomavirus (HPV).

Endometriosis- Causes, Symptoms, Diagnosis, Treatment
Endometriosis is a condition which causes growth of endometrium outside the uterus, It can cause severe pelvic pain, heavy bleeding and fatigue. It is closely associated with infertility.

The Menstrual Cycle:Phases- Follicular, Luteal, Ovulation and the Period.
The menstrual cycle begins on the first day of one period and ends before the first day of the next. It has 4 phases – the Period, Follicular, Ovulation and the Luteal Phase.





